Rick Davis Q&A
I’m a board-certified orthopedic surgeon, fellowship trained in hip and knee replacement. I attended medical school at the University of Cincinnati, followed by orthopedic surgery training at Mount Carmel Health in Columbus, Ohio. During my fellowship in Nashville, Tennessee at Southern Joint Replacement Institute, I received additional hands-on experience, focused both on first-time hip and knee replacements as well as the complex revisions that are sometimes required when older joint replacements wear out. I started my own practice in 2017.

Why should I consider a hip or knee replacement?
Hip and knee arthritis can cause a significant amount of pain, which can seriously limit your quality of life. Replacing the joint offers relief from that pain, helping you to get back to the lifestyle you enjoy.
You may want to watch our Premier Heath Joint Pain Webinar.
How do you determine if joint replacement is right for a patient?
Each patient has a different experience as they go through life and have to deal with their joint pain, so I really focus on individualized care. During your first visit I’ll typically start with a conversation to learn about your history and how joint pain is affecting your quality of life. Next, I’ll do an examination to see what limitations you may have around your hip or knee. We’ll also get some X-rays to determine the extent of any arthritis you may have, which I’ll review with you to help you understand exactly what’s causing your pain or other concerns. If surgery is an option, we’ll have a full discussion about the process, including the typical schedule, what your recovery will look like, what you can expect going forward, and answer any other questions you may have.
What is knee arthritis and what non-surgical options do I have?
 Knee arthritis, like other arthritis throughout the body, is simply when the nice, smooth cartilage we normally have in our joints wears out. In healthy bones, this cartilage allows for smooth movement as you walk or move. If the cartilage in your knee joint wears out, the bone surfaces that rub together become rough. This can cause pain and swelling and may also limit your range of motion.
Before undergoing a replacement, some patients benefit from non-surgical options like these:
Knee arthritis, like other arthritis throughout the body, is simply when the nice, smooth cartilage we normally have in our joints wears out. In healthy bones, this cartilage allows for smooth movement as you walk or move. If the cartilage in your knee joint wears out, the bone surfaces that rub together become rough. This can cause pain and swelling and may also limit your range of motion.
Before undergoing a replacement, some patients benefit from non-surgical options like these:
- Medication, including Tylenol or anti-inflammatories like ibuprofen
- Cortisone injections
- Gel or synthetic injections
- Platelet-rich plasma (PRP) or stem cell injections
What is a knee replacement, and how does it relieve pain?
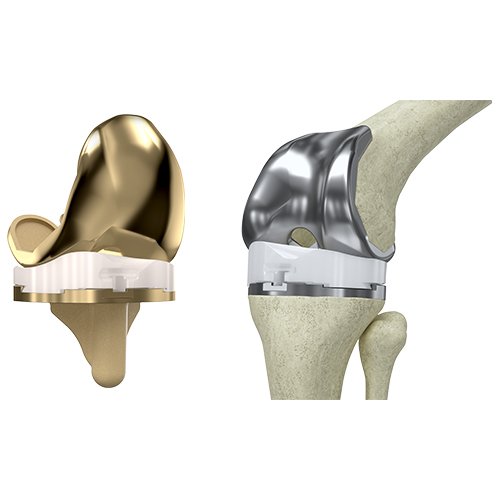 Knee replacement is simply a resurfacing of the end of your bone and your knee joint, which includes the femur (your thigh or upper leg bone) and the tibia (the larger bone in your lower leg). To perform the procedure, we make an incision directly down the center of the knee, remove the bad cartilage on the end of the femur and replace it with a metal cap. We also cement a metal tray at the top of your tibia, along with a plastic piece that locks in between. Your kneecap is then resurfaced with a plastic “button”on the underside of the bone. So, when you walk or bend your knee after the surgery, the joint moves smoothly again — it’s all metal-on-plastic parts. This relieves your pain because there are no nerve endings within the knee replacement. Nowadays, a knee replacement should last you 20 to 30 years.
Knee replacement is simply a resurfacing of the end of your bone and your knee joint, which includes the femur (your thigh or upper leg bone) and the tibia (the larger bone in your lower leg). To perform the procedure, we make an incision directly down the center of the knee, remove the bad cartilage on the end of the femur and replace it with a metal cap. We also cement a metal tray at the top of your tibia, along with a plastic piece that locks in between. Your kneecap is then resurfaced with a plastic “button”on the underside of the bone. So, when you walk or bend your knee after the surgery, the joint moves smoothly again — it’s all metal-on-plastic parts. This relieves your pain because there are no nerve endings within the knee replacement. Nowadays, a knee replacement should last you 20 to 30 years.
What is hip arthritis and what non-surgical options do I have?
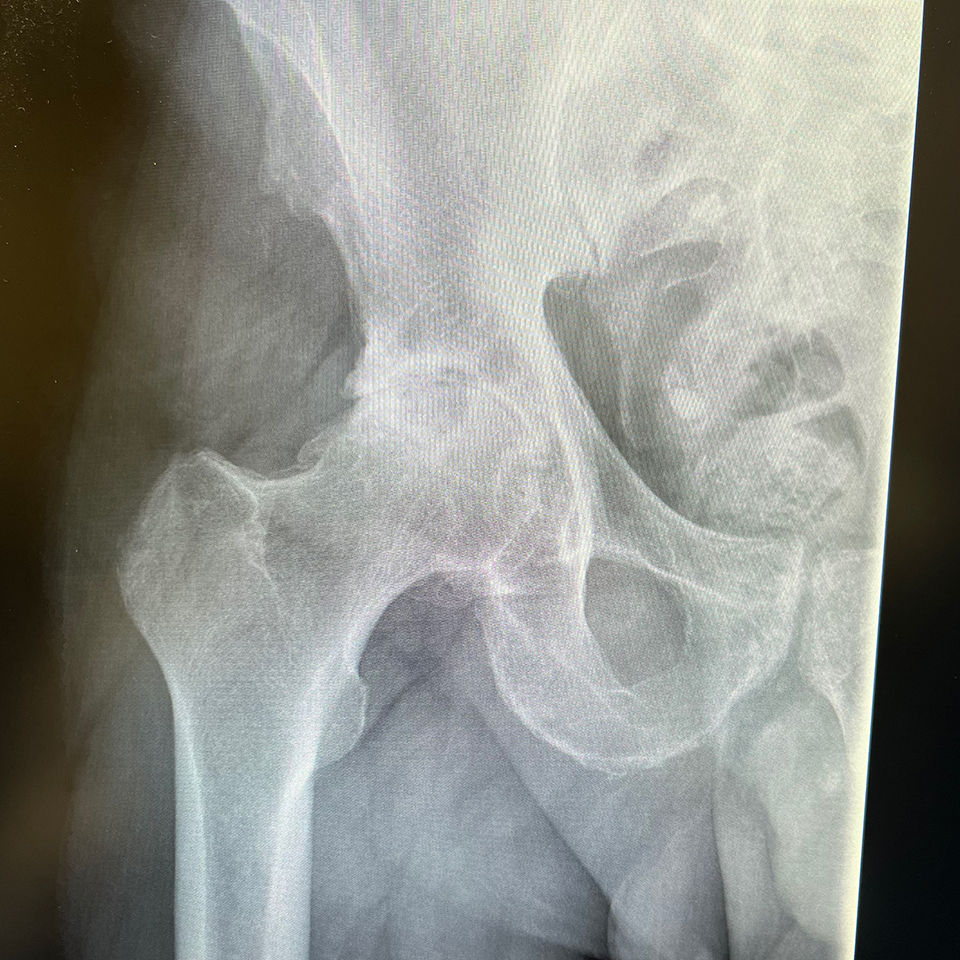 Similar to knee arthritis and other arthritis throughout your body, hip arthritis is caused when the smooth cartilage found in the hip joints wears out. Normally the cartilage in a hip joint allows for free motion and painless walking. In hip arthritis some or all of that cartilage is lost, creating rough surfaces. Bone starts to rub on bone, causing pain and inflammation.
Prior to any surgery, you can try treating hip arthritis with medication, such as Tylenol or anti-inflammatories like ibuprofen. Cortisone or joint injections can also help to decrease swelling and relieve pain.
Similar to knee arthritis and other arthritis throughout your body, hip arthritis is caused when the smooth cartilage found in the hip joints wears out. Normally the cartilage in a hip joint allows for free motion and painless walking. In hip arthritis some or all of that cartilage is lost, creating rough surfaces. Bone starts to rub on bone, causing pain and inflammation.
Prior to any surgery, you can try treating hip arthritis with medication, such as Tylenol or anti-inflammatories like ibuprofen. Cortisone or joint injections can also help to decrease swelling and relieve pain.
What is a hip replacement, and how does it relieve pain?
 A hip replacement can be performed through an incision directly in the front of your thigh or along the side. Either way the end result is the same. Damaged bone and cartilage are removed, a new cup is placed inside of your pelvic bone, and a plastic or polyethylene liner is locked inside of it. In addition, a metal stem with a ceramic head is fitted to the top of your thigh bone. When you walk or move your hip after surgery, your new hip replacement moves smoothly, eliminating the rubbing of rough bone that caused the pain and inflammation.
A hip replacement can be performed through an incision directly in the front of your thigh or along the side. Either way the end result is the same. Damaged bone and cartilage are removed, a new cup is placed inside of your pelvic bone, and a plastic or polyethylene liner is locked inside of it. In addition, a metal stem with a ceramic head is fitted to the top of your thigh bone. When you walk or move your hip after surgery, your new hip replacement moves smoothly, eliminating the rubbing of rough bone that caused the pain and inflammation.
How do you minimize pain after surgery?
There have been many advances in what we call the perioperative (during and after your surgery) pain control. This actually begins before your surgery. We typically use a spinal anesthesia, which is kind of like an epidural that numbs your legs from the waist down. Although you’ll still be asleep, you won’t have to be intubated or tubed. This allows you to wake up quicker and decreases your pain after the surgery. The anesthesiologist will also give you pain-reducing medications during the procedure.
While you’re still asleep but after the joint replacement is performed, I’ll inject a local anesthetic (numbing medicine) into the tissue around the hip or knee, which helps to suppress most of the pain you would otherwise experience in the first 36 hours. This allows you to stand up on the same day of surgery, walk with a physical therapist, get home, and stay as comfortable as possible during the first night into the next day. We’ll also send you home with an ice pack machine, anti-inflammatories if you’re allowed to take them, plus a pain-relieving medication or narcotic you can take if you need during your recovery.
What’s the typical recovery time after a knee replacement?
The total recovery time is typically about three months, and I often describe these in a few different phases:
The first two weeks after a knee replacement are what I tend to call the “What did I get myself into?” phase. It’s normal to have quite a bit of soreness from the surgery during this time. This is where that ice pack machine comes into play — it really helps with your swelling — along with anti-inflammatories and sometimes pain medication as well. After you get past that first two weeks, your pain level typically goes down week by week.
For the first six weeks you’ll visit a physical therapist’s office — that’s about how much time it takes to get your full range of motion back. At the end of that time, you can start getting back to just about any activity you like.
I’ll see you in the office two weeks after the surgery, and then again at six weeks. If you have a desk job, you can typically go back to work after six to eight weeks. If your job involves manual labor where you’re up and walking throughout the whole day, it’s about a three-month time period.
What’s the typical recovery time after a hip replacement?
Hip replacement recovery usually takes about three months. As with knee replacements, the first two weeks are typically when you’ll have the most soreness from post-surgery pain. This can be relieved using an ice pack, anti-inflammatories, and pain pills if you need them.
After the first two weeks, you can begin easing away from using a walker, possibly supporting the new hip with a cane for a week or so. By week three or four you’ll typically be able to walk on your own again. Usually by week six you can get back to anything you want to do.
Patients who work at a desk job or want to get back to a simple activity can typically return to work anywhere from three to six weeks after surgery. If you’re going back to a manual labor job you’ll typically need six weeks to three months after surgery before you return.
Can I go home the same day I have surgery?
Yes, and I encourage all my patients to do so. Thanks to the latest advances in anesthesia and pain control, including nerve blocks and medications, patients can go home the same day and be more comfortable than they would be in a hospital room. We’ll get you up walking with a physical therapist on the same day as your surgery so they can go over different tips and tricks for getting around your home. You’ll get to sleep in your own bed, eat your own food, and benefit from family support.
Is there any advantages to robotic-assisted surgery?
As an orthopedic surgeon specializing in joint replacement, I do both non-robotic as well as robotic-assisted knee replacement. Either way patients do well and regain their quality of life.
There are some common misconceptions about what robotic-assisted surgery is. The robot doesn’t do the surgery for you — the surgeon guides the robotic arm through the entire procedure. Although the robotic system helps me to position surgical instruments more precisely, I’m still the one who actually makes all of the cuts.
Studies have shown that robotic-assisted surgery can reduce blood loss and post-surgical discomfort, which are both significant advantages. Whether robotic-assisted surgery is right for you is part of the discussion we’ll have when we go over our surgical plan.
Will I need physical therapy after a hip or knee replacement?
Physical therapy is a vital part of your recovery. Typically, you’ll have your first appointment with a physical therapist in their office within a day or two after your surgery. This allows you to get up, move and get walking again faster, which enables you to get back to your life sooner. Another benefit is that your physical therapist can help decrease swelling around your surgery site. They’ll also assist you with techniques for getting around that will help you recover in less time.
Do I need to see my primary care physician or other specialty doctors before the surgery?
Prior to hip or knee replacement, I’ll ask you to see your primary care physician. They know your medical history best and can give us guidance if there’s any additional lab work or tests that need to be done. If you see other specialists, such as a cardiologist or heart doctor, we’ll typically ask you to see them as well to make sure your heart and so forth are safe to undergo surgery.
Are there any conditions that could prevent me from having surgery?
In most cases we can work with your primary care physician or other specialists to ensure you’re in sufficiently good health before surgery. The most common conditions that cause concern are excessive weight and nicotine use.
Many recent studies have found that a high body mass index (BMI) increases a patient’s risk of complications after surgery. In such cases I’ll have a discussion with you about safe ways to lose weight and get down to a healthier BMI before you undergo surgery.
Studies have also found that nicotine use can decrease your skin’s ability to heal, which can potentially cause infection. If you’re a smoker, there are many strategies to help you to quit smoking prior to surgery. I’ll counsel you and, if needed, consult with your primary care physician about medications that can decrease your cravings. There are also nicotine patches and other treatment options. This is a very important part of the planning prior to hip or knee replacement and will help to get your body as healthy as possible prior to undergoing surgery.
What is revision (or reoperation) hip or knee replacement?
Revision is a repeat operation on a previously replaced joint. For example, if a patient had a knee replacement 20 to 25 years ago, the components could start to wear out over time, causing pain and swelling. A revision is simply a procedure to remove the worn parts and replace them with new ones that should last you an additional 20 to 30 years.
Hip replacement parts can also wear out over time. As with knee revision, hip revision is simply a procedure to remove the old parts and put in new hip replacement parts that should last you for many years to come.
What are the signs that I might need a reoperation?
If you had a previous hip or knee replacement years ago, pain that wasn’t there before, swelling in the joint, or new discomfort may be signs that your parts are wearing out. If this is the case, I’ll perform an evaluation and have a discussion with you about your options.
When can I get back to work?
This is probably the most common question I’m asked. The answer depends on the type of job you do.
After a knee replacement, if you have a desk job or do some other type of work where you don’t have to do a lot of walking, you can get typically go back to work in the 6-to-8-week range. If you’re going back to a manual labor job where you need to be on your feet throughout the day, it will probably be a good three months before you’re getting back to that job full time.
From a hip replacement standpoint, you can usually get back to a desk job anywhere from two to four weeks after surgery. If you’re going back to a manual labor job, you’ll usually need at least six weeks after surgery — sometimes up to three months depending on the demands of your job.
Are there differences between implant designs from different companies?
There are many different implant manufacturers nowadays, which is great because it means patients have a lot of options. I take a very patient-centered approach, so we tailor which implant we use to whatever best fits your needs. For example, some implants are designed for people who are very, very active and still want to do things that younger people do. There are also more patient-specific types of implants, especially for those requiring a revision surgery. We’ll discuss your options as part of your evaluation, and I’ll actually show you models of different implants to help you determine which one is right for you.
What are the implants made of?
Knee replacements are typically made of cobalt chrome or titanium. Some implants also have a ceramic coating. Between the two parts on the femur and the tibia is a plastic piece made from highly cross-linked polyethylene.
Hip replacement implants are typically made of titanium. There’s also a plastic or a polyethylene liner that sits inside of the acetabular, or cup part in your pelvis. The head that attaches to the top of the femur implant is typically either metal or ceramic.
Could I be allergic to the metals? If so, do I have other options?
This is very rare but can be identified before surgery with a few simple screening questions. If we have a concern, we’ll take a blood sample and evaluate it with lab work prior to any joint replacement.
What are my restrictions after surgery?
In general, I don’t restrict my patients from doing much. I don’t recommend running marathons on new joint replacements because it can cause them to wear out a little quicker. Apart from that I encourage you to get back to any type of sport or other activity you like. You can play basketball, play tennis, golf, go on hikes, ride your bicycle and things like that. I prefer you to be active so that you stay healthy and enjoy your life after your joint replacement.
How long do implants last? Will I ever need another surgery?
Hip and knee replacements have become more durable in recent years. In the past it was common for them to last anywhere from 5 to 10 years, but they’ve come a long way since then. New advances in joint technology, specifically with advances in the polyethylene or plastic piece, now enables them to last 20 to 30 years — possibly even longer.

